December 2016 - Volume 33 - Issue 12 - p 881–897
doi: 10.1097/EJA.0000000000000533
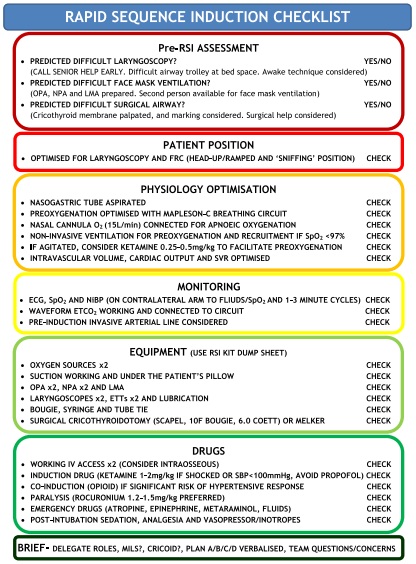
Emergency anaesthesia is an important therapeutic measure in out-of-hospital emergency medicine. The associated risks are considerably higher than those of in-hospital anaesthesia. The primary objectives of emergency anaesthesia are hypnosis, analgesia, oxygenation and ventilation through airway management. The secondary objectives of emergency anaesthesia are amnesia, anxiolysis, the reduction of oxygen consumption and respiratory work, the protection of vital organs and the avoidance of secondary myocardial and cerebral damage. A critical evaluation of the indications for out-of-hospital emergency anaesthesia must take into consideration patient, case and provider-related factors. Rapid sequence induction of emergency anaesthesia includes standard monitoring, preoxygenation, standardised preparation of emergency anaesthesia, drug administration, manual in-line stabilisation during intubation (if necessary), airway management and checking of correct tube placement. Spontaneously breathing casualties should receive preoxygenation for at least 3 to 4 min with a tight-fitting facemask with reservoir using 12 to 15 l min_1 of oxygen or with a demand valve providing 100% oxygen. As an alternative, preoxygenation may be performed as noninvasive ventilation with 100% oxygen. Standardised anaesthesia preparation comprises filling drugs into syringes and labelling them, checking ventilation equipment, preparing endotracheal tube and syringe for inflating the cuff and the introducer, stethoscope and fixation material, preparing alternative instruments for airway management as well as checking suction, ventilation and standard monitoring devices, including capnography. Standard monitoring for out-of-hospital emergency anaesthesia comprises ECG, blood pressure measurement and pulse oximetry. Continuous capnography is always and exclusively performed to check the placement of airway devices, as well as to indirectly monitor haemodynamics.



 RSS Feed
RSS Feed