Emerg Med J doi:10.1136/emermed-2014-204466 (published online first)
Anesthesiology. 2015 Feb;122(2):448-64
Abstract Care of burn-injured patients requires knowledge of the pathophysiologic changes affecting virtually all organs from the onset of injury until wounds are healed. Massive airway and/or lung edema can occur rapidly and unpredictably after burn and/or inhalation injury. Hemodynamics in the early phase of severe burn injury is characterized by a reduction in cardiac output and increased systemic and pulmonary vascular resistance. Approximately 2 to 5 days after major burn injury, a hyperdynamic and hypermetabolic state develops. Electrical burns result in morbidity much higher than expected based on burn size alone. Formulae for fluid resuscitation should serve only as guideline; fluids should be titrated to physiologic endpoints. Burn injury is associated basal and procedural pain requiring higher than normal opioid and sedative doses. Operating room concerns for the burn-injured patient include airway abnormalities, impaired lung function, vascular access, deceptively large and rapid blood loss, hypothermia, and altered pharmacology. Scand J Trauma Resusc Emerg Med. 2014 Sep 11;22(1):41.
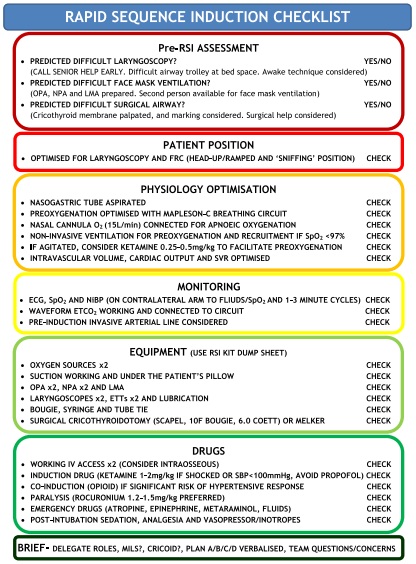
Introduction Rapid sequence induction (RSI) of critically ill patients outside of theatres is associated with a higher risk of hypoxia, cardiovascular collapse and death. In the prehospital and military environments, there is an increasing awareness of the benefits of standardised practice and checklists. Methods We conducted a non-systematic review of literature pertaining to key components of RSI preparation and management. A standard operating procedure (SOP) for in-hospital RSI was developed based on this and experience from large teaching hospital anaesthesia and critical care departments. Results The SOP consists of a RSI equipment set-up sheet, pre-RSI checklist and failed airway algorithm. The SOP should improve RSI preparation, crew resource management and first pass intubation success while minimising adverse events. Conclusion Based on the presented literature, we believe the evidence is sufficient to recommend adoption of the core components in the suggested SOP. This standardised approach to RSI in the critically ill may reduce the current high incidence of adverse events and hopefully improve patient outcomes. JAMA. 2015;313(5):471-482. doi:10.1001/jama.2015.12.
Importance Severely injured patients experiencing hemorrhagic shock often require massive transfusion. Earlier transfusion with higher blood product ratios (plasma, platelets, and red blood cells), defined as damage control resuscitation, has been associated with improved outcomes; however, there have been no large multicenter clinical trials. Objective To determine the effectiveness and safety of transfusing patients with severe trauma and major bleeding using plasma, platelets, and red blood cells in a 1:1:1 ratio compared with a 1:1:2 ratio. Design, Setting, and Participants Pragmatic, phase 3, multisite, randomized clinical trial of 680 severely injured patients who arrived at 1 of 12 level I trauma centers in North America directly from the scene and were predicted to require massive transfusion between August 2012 and December 2013. Interventions Blood product ratios of 1:1:1 (338 patients) vs 1:1:2 (342 patients) during active resuscitation in addition to all local standard-of-care interventions (uncontrolled). Main Outcomes and Measures Primary outcomes were 24-hour and 30-day all-cause mortality. Prespecified ancillary outcomes included time to hemostasis, blood product volumes transfused, complications, incidence of surgical procedures, and functional status. Results No significant differences were detected in mortality at 24 hours (12.7% in 1:1:1 group vs 17.0% in 1:1:2 group; difference, −4.2% [95% CI, −9.6% to 1.1%]; P = .12) or at 30 days (22.4% vs 26.1%, respectively; difference, −3.7% [95% CI, −10.2% to 2.7%]; P = .26). Exsanguination, which was the predominant cause of death within the first 24 hours, was significantly decreased in the 1:1:1 group (9.2% vs 14.6% in 1:1:2 group; difference, −5.4% [95% CI, −10.4% to −0.5%]; P = .03). More patients in the 1:1:1 group achieved hemostasis than in the 1:1:2 group (86% vs 78%, respectively; P = .006). Despite the 1:1:1 group receiving more plasma (median of 7 U vs 5 U, P < .001) and platelets (12 U vs 6 U, P < .001) and similar amounts of red blood cells (9 U) over the first 24 hours, no differences between the 2 groups were found for the 23 prespecified complications, including acute respiratory distress syndrome, multiple organ failure, venous thromboembolism, sepsis, and transfusion-related complications. Conclusions and Relevance Among patients with severe trauma and major bleeding, early administration of plasma, platelets, and red blood cells in a 1:1:1 ratio compared with a 1:1:2 ratio did not result in significant differences in mortality at 24 hours or at 30 days. However, more patients in the 1:1:1 group achieved hemostasis and fewer experienced death due to exsanguination by 24 hours. Even though there was an increased use of plasma and platelets transfused in the 1:1:1 group, no other safety differences were identified between the 2 groups. Trial Registration clinicaltrials.gov Identifier: NCT01545232 |
Categories
All
Archives
October 2021
|
 RSS Feed
RSS Feed